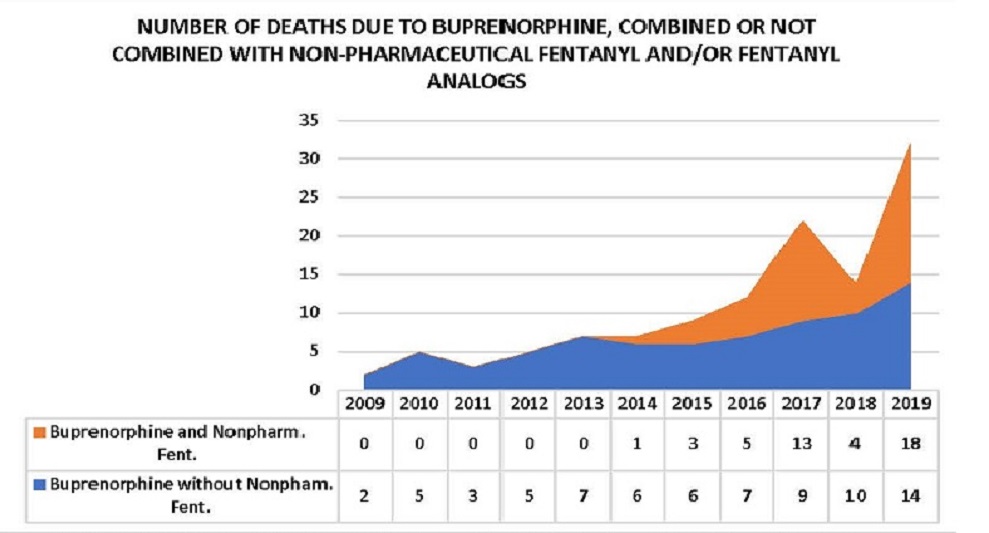
I wrote a controversial post (see below) in the end of 2019 as prescribing practices in Maine underwent a seismic shift allowing patients not yet stabilized on suboxone to receive seven to thirty day prescriptions without the SAMHSA recommended accompanying psychosocial treatment per the DATA 2000 guidelines. Harm Reductionists, of which I have been one since 1979, defended the rights of the patient to choose their method of treatment and their level of engagement. From a social justice perspective, this makes perfect sense. Honoring the philosophy of meeting a person where they are without compromising their dignity. However, the divide between rational, humane thinking by well intentioned physicians and medication motivated patients seeking relief is sometimes catastrophic. Numbers do not lie. The reality of the outcomes to this model is clearly illustrated by the buprenorphine mortality data released today by the Maine Attorney General’s Office. Buprenorphine mortality data indicates a 129% increase of buprenorphine related overdoses in 2019 over 2018.
I have always believed that the degree of variance between the real and the ideal is closely correlated with the degree of cognitive dissonance that one experiences. This paradigm can also be applied to medication dispensing standards for opioid use disorder treatment. The ideal in this scenario is that all opioid dependent persons seeking treatment will be appropriately motivated and have the social supports to succeed in Medication Assisted Treatment without psychosocial supports. The reality is that treatment retention, rates of incarceration and mortality statistics tell a different story. It is common knowledge on the street that many individuals sell most of their prescription and use the proceeds to purchase their drug of choice which lately has been Fentanyl due to the scarcity of undiluted heroin in our region.
It is my belief based upon my personal lived and professional experience that closely monitored medication dispensing during the initial physiological and behavioral stabilization period is critical to not only reducing mortality but increasing the probability of sustained recovery. We have moved well beyond the disease model originally put forth regarding alcoholism by E.M Jellinek in 1946. Yes, tremendous advances have been made in neuroscience regarding the impact of acute and chronic opioid use however addiction is a psychobiosocial disorder and treatment with medication only addresses only the biological component. There are no magic bullets and therefore the incidence of addictive disorders will only escalate until the medical and clinical professions can work together to adopt a uniform definition of best practices. As Gabor Mate, a renowned addiction and trauma expert states, “It is impossible to understand addiction without asking what relief the addict finds, or hopes to find, in the drug or the addictive behavior”. Neither buprenorphine, methadone not naltrexone will supply that answer but rather postpone the necessity for the question to be answered.
December 21, 2019: Facebook Post
“We as a society have been in search for a magic bullet to treat opioid use disorders since the early 70’s. Medication assisted treatment although essential in acute and chronic OUD’s to abate craving and elevate dopamine levels is most often not sufficient unto itself as addiction is a psychobiosocial disorder. Unfortunately, in our attempt to reduce the incidence of opioid mortality many well intended practitioners now are addressing only the biological component of addiction and dispensing medication, especially suboxone, without the appropriate level of accompanying psychosocial treatment. This practice is rampant in Maine and contributes to the overdose mortality rate from continued illicit opioid use due to diversion as a result of loose prescribing practices. To expect an individual addicted to heroin or fentanyl who is in a pre-contemplative state motivationally and has limited if any social supports to responsibly self-administer daily a seven-day prescription of a partial agonist orally with negligible euphoric effects and abandon the behavior and lifestyle of the street without structured psychosocial treatment is not only naive but negligent”


Leave A Comment